This demanding project migrated complex cancer patient data from a large oncology practice’s legacy system into an existing instance of Epic at a major academic medical center (AMC).
We have migrated millions of patient records and can guide you through the process—we know how to handle the large volumes of data, complex technical requirements, and disparate document types. Our careful planning, phased execution, and attentive support help our clients avoid arduous manual abstraction, last-minute scope changes, and unpleasant surprises at go-live. We are excited to help you simplify and de-risk your specialty data conversion initiative—get in touch and we’ll help you get back to focusing on what matters most!
The Clients: Merging Leaders in their Fields
The Specialty Practice:
- Prestigious multi-location oncology practice helping patients fight cancer and manage their hematology disorders for over 35 years
- 41,000 patients across 7 facilities (clinics and infusion centers) before joining the larger healthcare system
- QOPI Certified Practice, demonstrating quality and safety in the administration of cancer care
The Academic Medical Center:
- Top-ranked teaching hospital and cancer center with a history dating back 110 years, known for early adoption of clinical technology
- Leader in transplant results and innovation, achieving many of the field’s “firsts” and maintaining strong outcomes
- Strategic roadmap included connect with patients before they present at the ER, treating them sooner, and helping them avoid the ER
The Situation: Complex Legacy-to-Epic Data Conversion
The oncology practice needed to integrate their IT systems as part of joining the larger health system, and they wanted to do it in a way that left no doubts about how providers would find the information they needed on day one.
They needed to make sure their thousands of patient records from the legacy oncology-specific system would be available and accurate when they started using an already-live instance of Epic’s electronic health record (EHR).
This is harder than it sounds, because the intricate nature of cancer care generates complex data, which doesn’t automatically map to the new system’s data structure.
The Solution: Transparency and Expertise
To guarantee their success, we worked with each provider to understand their workflows and convert as many data elements as possible.
The HDM team met regularly with providers and used transparent processes for scoping, mapping, validation, and testing.
This allowed us to maintain provider engagement, provide hands-on training, and ensure our data conversion process yielded consistent workflows in the new EHR—all of which led to a smooth go-live without surprises. Our experience gives us the confidence to help our clients navigate the complexity and avoid common obstacles:
- Conflicting lab result formats
- Documentation for lab orders and treatment plans
- Key therapeutic data unlinked to clinical episodes, creating timeline discontinuities
- Missing care team records
The Details: Interfaces and ETL Processes
First, meeting with providers to discuss what historical data was essential for patient care allowed us to refine the project scope before beginning the migration, saving time by avoiding unnecessary rework.
We identified which elements would use common HL7 interfaces and which would require specific extract, transform, load (ETL) processes to convert into Epic.
For this client’s legacy system and interfaces, our technical experts determined the best path for each data element and how to format it during extraction. For example, we used the Incoming Results interface to load historical lab results – no surprises there – but we had to get creative with nonstandard items and legacy system reports. We also did a lot of detail work to convert medication history, which causes difficulties because of the need for reconciliation (“med rec”), but it’s too important to omit for cancer treatment records.
To get patient data ready for migration to the new system, we extracted from the legacy system, and used a staging database to transform it to align with Epic data load standards.
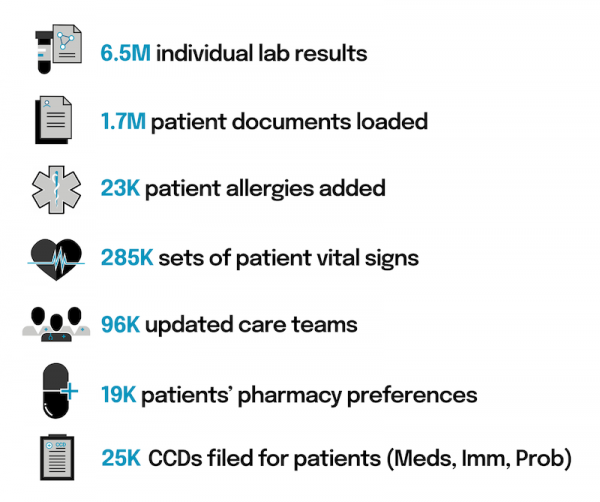
What does a data conversion look like for 41,000 patients?
Data governance and data integrity are crucial during these processes, because of periodic data load updates and the potential consequences of errors. If ETL practitioners have not mastered this discipline, they can cause issues like duplicate records or decimal place errors, which can have disastrous real-world consequences for patient safety if they occur in a production environment. To maintain data integrity, we meticulously test data loads for accuracy and completeness in a safe Epic environment. Rigorous testing strategies are built into every engagement.
We also guided providers through validating their own patient data in the safe Epic environment, making sure physicians and clinical staff saw the data they expected. Our approach to validation is both thorough and efficient, maximizing clinicians’ input while respecting their time. We give end users as much access as possible throughout each phase.
The Result? Success
The exhaustive testing and validation we conducted was rewarded with an exceptionally smooth go-live.
Most data conversion vendors can’t support physicians at go-live, but HDM is a full-service healthcare IT firm, and we provided this oncology practice with attentive, individualized support, answering questions, orienting providers to the system, monitoring error queues, and working closely with the command center.
We did this to make sure not only that we got the high-stakes data converted correctly, but also that our clients were happy with the outcome.
For questions about this data conversion you can contact the author, Jacob Zubler, here:
HDM’s Transplant Data Conversion projects
Connect with Jacob
jacob.zubler@healthdatamovers.com

